PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
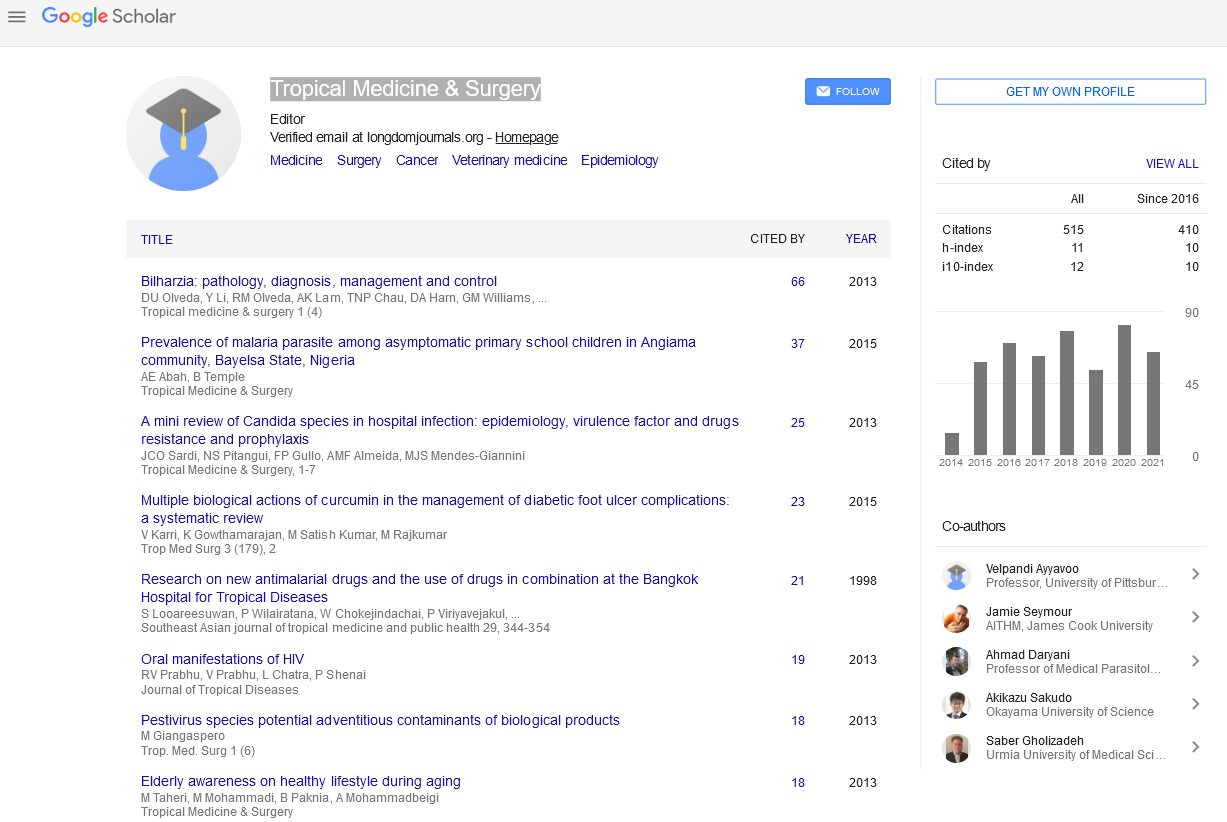
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
How to Implement a Small Blood Bank in Low and Middle-Income Countries Work in Progress?
Pierre Zachee* and Philippe Vandekerckhove
Compared to High-Income countries (HIC), a shortfall in the provision of blood remains a multifaceted problem in Low and Middle-Income Countries (LMIC) with a direct negative effect on clinical care. The reasons are multifactorial: not only lack of knowledge, skills, and resources, but also huge differences in environment climate, endemic transfusion transmittable infections, clinical set-up, availability of clean water, electricity. It is therefore obvious that simple translation of guidelines, standards, experiences, and the total organization from HIC to LMIC is not the best way to proceed. Adapted, but not less adequate methods for blood transfusion training, organization, and accreditation are required. The Global Advisory Panel (GAP) already formulated an adapted specific answer in terms of training and accreditation. But this is not enough. Academic centres, the GAP, countries, non-governmental organizations, and others need to test current and innovative diagnostic, production, and storage methods in a joint venture with the industry. Also, medical decisions focused on transfusion must be tested before implementation in facilities allowing pre-qualification of tests and devices. The entire transfusion chain needs to be simulated in a competence and training centre, focusing on the region where it will be applied. One of the renowned tropical institutes, currently fulfilling all these requirements could be the ideal place for such a competence centre. This review highlights this and suggests possible ways and solutions.
Published Date: 2020-05-27; Received Date: 2020-05-03