Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
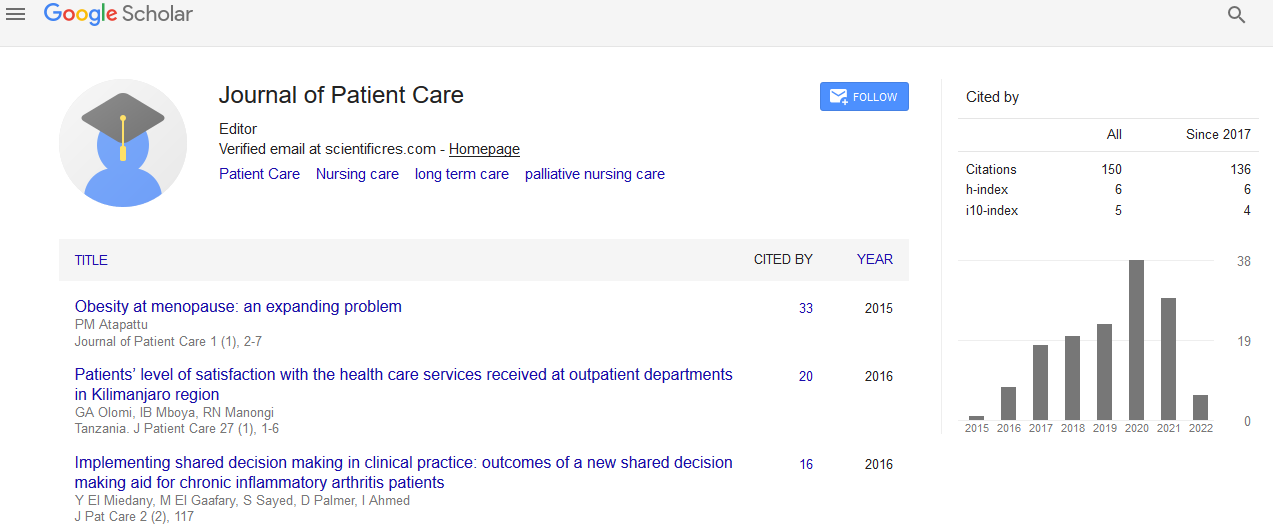
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Guided Imagery Intervention does not Affect Surgical Outcome of Patients Undergoing laparoscopic Cholecystectomy: A Multi-Centre, Randomised Controlled Study
Pijl AJ, de Gast HM, Jong M, Hoen MB, Kluyver EB, van der Vegt MH, Kanhai SRR and Jong MC
Objective: To investigate if a “non-pharmacological” intervention with guided imagery could reduce postoperative analgesic consumption, pain perception and preoperative anxiety, compared to standard care, in patients undergoing laparoscopic cholecystectomy (LC).
Methods: A randomized controlled study with two parallel groups was performed at two hospital departments of anesthesiology. A total of 140 patients (≥ 18 years) that were scheduled for LC were randomized to either receive guided imagery (N=70) or standard care instructions (N=70) as a control group. Patients in the guided imagery group were provided a CD to practice guided imagery once a day, 7 days prior to surgery. Primary outcome measurement was post-operative analgesic consumption. Secondary outcomes were preoperative anxiety, post-operative self-rated pain, patient satisfaction and adverse events.
Results: Of 140 patients that were randomized, 95 patients completed the study, 43 in the guided imagery group and 52 in the control group. Both groups were comparable at baseline with respect to demographic data. Compliance with intervention was fairly good as 77% of the patients had listened to the CD according to instructions. No significant differences (p=0.34) were observed for postoperative morphine use between the intervention (15.8 ± 18.5 mg) and control group (12.5 ± 13.6 mg). Secondary outcomes such as preoperative anxiety (APAIS: 15.2 ± 5.9 vs. 16.4 ± 5.9; p=0.36)), postoperative pain (VAS: 3.4 ± 1.8 vs. 3.0 ± 1.8; p=0.31) and patient satisfaction (PSQ: 4.1 ± 0.9 vs. 3.9 ± 0.8; p=0.47) also demonstrated no significant differences. No adverse events were reported in both groups.
Conclusion: A short preoperative guided imagery intervention demonstrated no additional beneficial effects compared to standard care for patients undergoing LC. It therefore seems not to be as simple as to provide patients with a CD before surgery in order to effectively self-manage postoperative pain.