PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
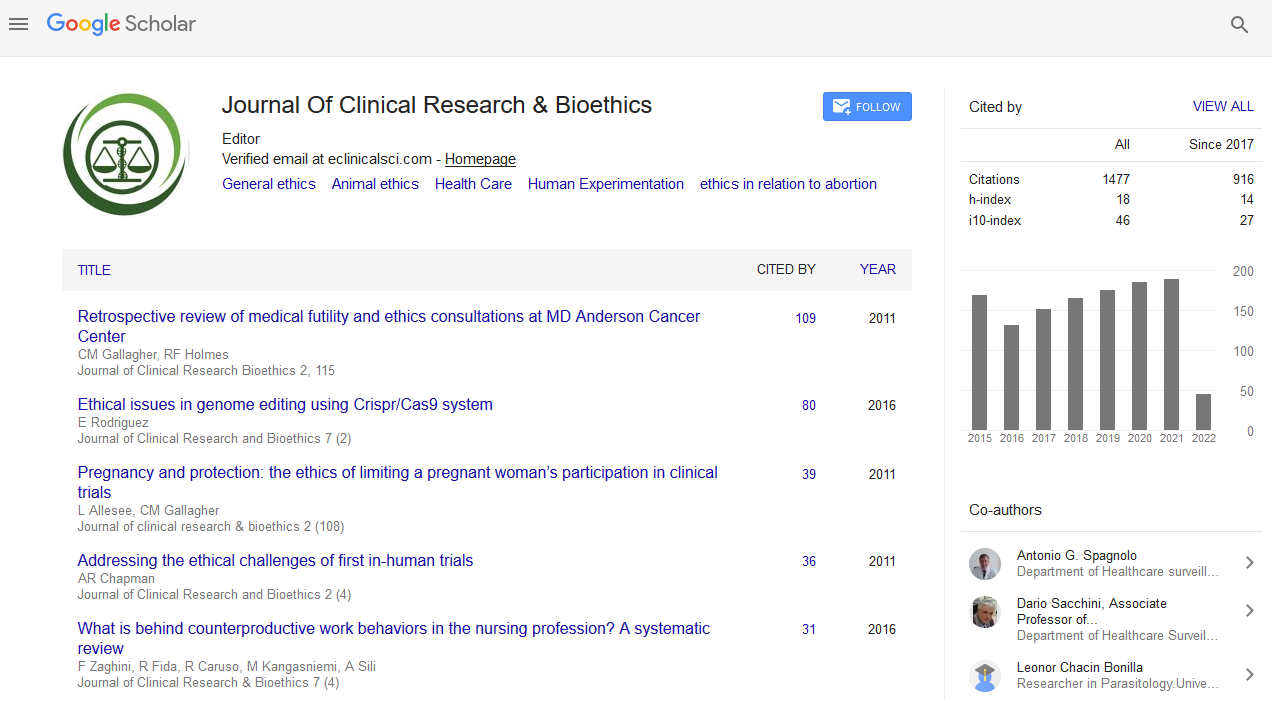
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Ethical Analysis of Medical Futility in Cardiopulmonary Resuscitation
Cardiopulmonary Resuscitation (CPR) is a life-saving intervention in emergency medical care practiced globally for the last more than seven decades. It cannot be a solution to prevent every death and there are risks associated with this intervention. This article focuses on the ethical dilemmas related to the decisions of medical futility in cardiopulmonary resuscitation particularly in emergency settings. There are guidelines for the decisions to start and stop CPR but are mostly based on technical grounds only. Technically possible interventions are not always medically reasonable and all four principles of biomedical ethics - viz. respect for autonomy, beneficence, non-maleficence and justice are associated with the issues of medical futility in this process. Autonomy deals with the issues of the individual right for CPR as well as the other side of the coin do-not-resuscitate (DNR) including death with dignity. The ‘advance directive’ and the need for surrogate consent are further dimensions of autonomy. As a life saving measure, beneficence comes into play while non-maleficence argues against performing CPR when the outcomes are harmful or futile. Futile interventions have to be avoided for the justice so that the precious intensive care units are not occupied waiting for the end-of-life. Literatures were reviewed and analyzed in the context of medical futility in CPR and the ethical dimensions of the issues have been explored. Ethical approach assists in deciding the futility of cardiopulmonary resuscitation in a given situation where the shared decision is taken by the medical professionals and the surrogates of the patients.