Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
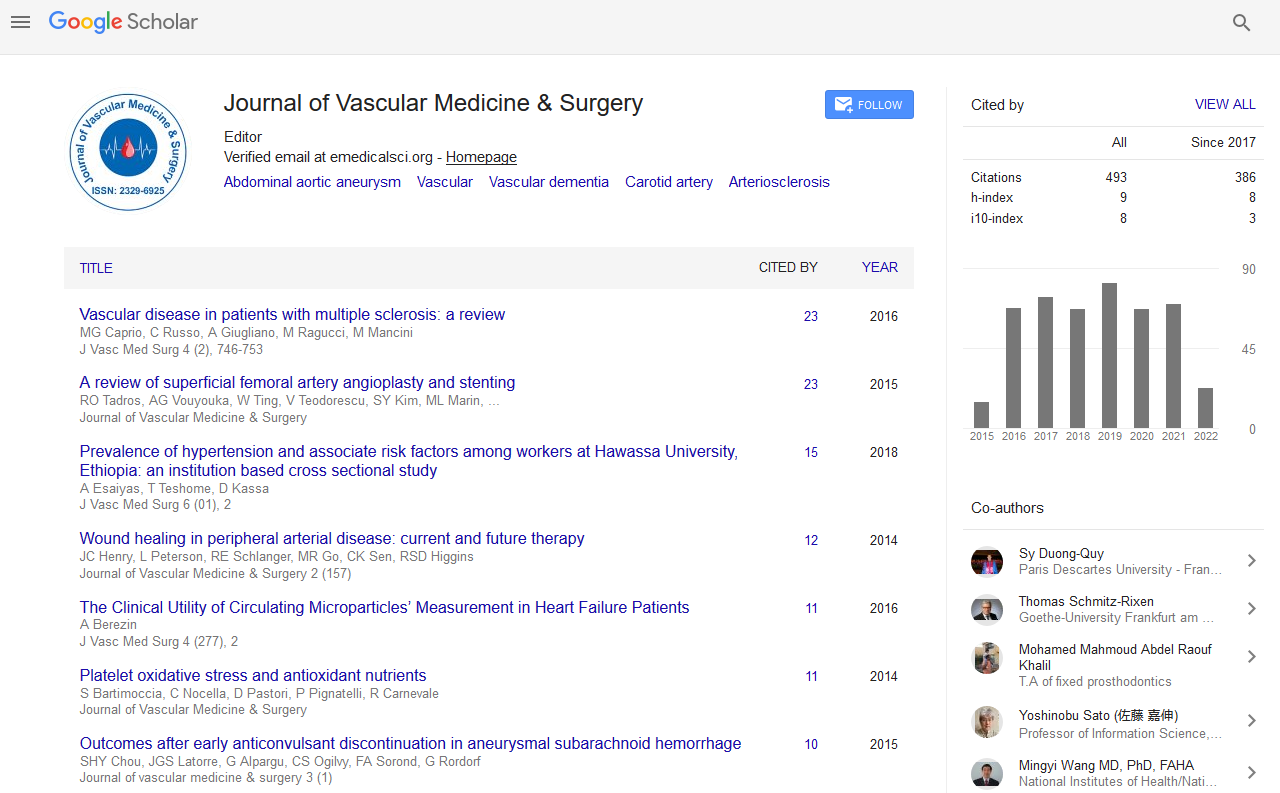
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Endovascular Limb Salvage for Haemodialysis Patients-A Retrospective 10-Year Review
Adam Tam*, Anastasia Benjafield, Rachel Barnes, Andrew EdwardS
Objectives: Endovascular revascularization is a commonly used method for limb salvage in haemodialysis patients with chronic limb threatening ischemia (CLTI). The aim of this study was to determine the long-term limb- and survival outcomes in this highly co-morbid population. Methods: A single center, retrospective review of all endovascular procedures performed for limb salvage from 1/2010-1/2020 was undertaken. Inclusion criteria were patients on haemodialysis, presenting with infra-inguinal peripheral vascular disease resulting in CLTI. CLTI was defined as ischaemic pain at rest or the presence of tissue loss. The primary outcome measure was limb salvage at 30 days, 1, 2 and 3 years. The secondary outcome measures were amputation free survival and all-cause mortality along the same time periods. Results: 39 patients (mean age 69.8 years) underwent 47 endovascular procedures. Mean length of follow-up of 24.8 ± 26.9 months. EVT indication for tissue loss was 80.7%. Limb salvage rate at 30-days, 1 year and 3 year limb salvage was 87.2%, 76.9% and 74.4%. Mortality at 30-days, 1 year and 3 years was 17.9%, 51.3% and 69.2%. One year amputation-free survival was poor at 48.7%. Patients undergoing minor amputations <30 days after EVT were more likely to have a major amputation (OR 2.4, 95% CI 0.17-32.8). Partial or unsuccessful angioplasty did not increase the risk of major amputation (OR 1.03, 95% CI 0.22-4.68). Conclusion: EVT is safe and has adequate limb salvage outcomes. However mortality in this group is high, reflecting the co-morbid nature of this patient cohort when presenting with CLTI. Patients undergoing debridement or minor amputation <30 days from EVT have a higher risk of major amputation. Further research is required to determine factors affecting survival within this population to allow appropriate patient selection for EVT.
Published Date: 2021-04-30; Received Date: 2021-04-01