Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Euro Pub
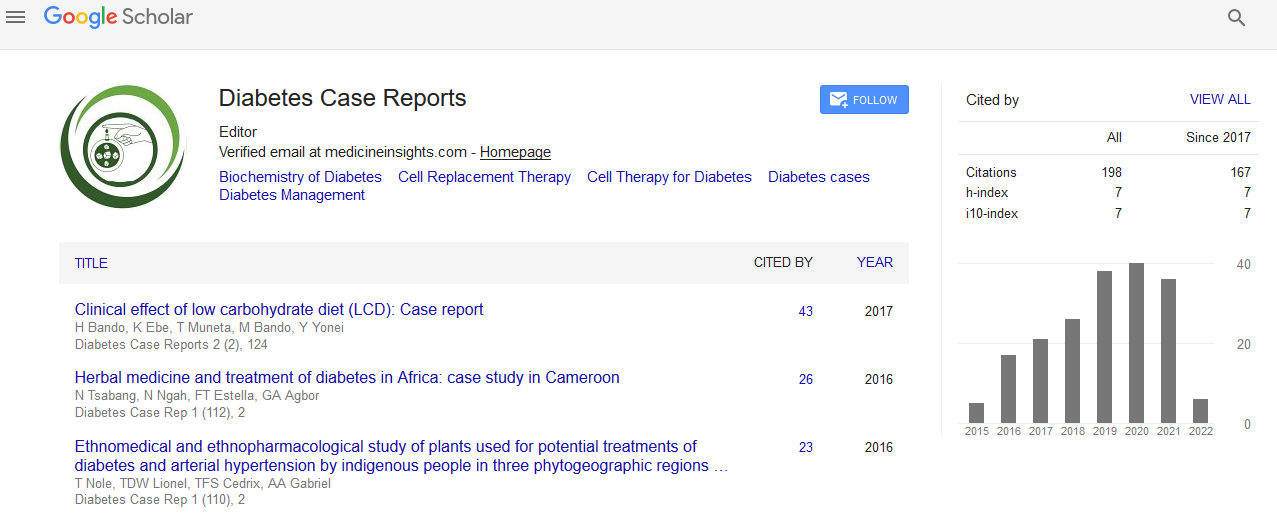
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Endocrinology 2018: Differential diagnosis between iodine-induced hyperthyroidism and non iodine-induced hyperthyroidism with computed tomography - Ramchandra Sargar - RUDN University, Russia
Ramchandra Sargar
Background: In hyperthyroidism, physician must have information that whether this hyperthyroidism is caused due to excess iodine or not, as this fact dramatically affects on the prognosis and management of subsequent therapy. The diagnostic methods which are nowadays widely used like, serum TSH level, fT4, fT3 and USG of thyroid gland, do not answer to the question of what is the pathogenesis of hyperthyroidism in terms of iodine induction. Thyroid scintigraphy or scan with technetium (99mTc) allows assessing only in non-iodine induced hyperthyroidism by diffused uptake. Thyroid scintigraphy, in case of iodine induced hyperthyroidism, will not allow visualizing thyroid gland due to blocked function of iodine trapping (Wolff-Chaikoff effect). This blockade can occur not only due to Wolff-Chaikoff effect, but also some elements like, bromide and corvalol etc. Patients might not remember about these elements, which particularly reduce the value of DD in hyperthyroidism with thyroid scintigraphy. In accentuation, the only method, which allows diagnosing the thyroid function disorder, is the thyroid density imaging with computed tomography, so called Hounsfield unit (HU). This thyroid density is directly proportional to the concentration of intrathyroidal stable iodine. Based on literature data, the following variations of the thyroid density in HU are proposed for all regions of Russia, reflecting the euthyroid state is from 85 to 140 HU. When there is iodine-induced impairment of thyroid function, thyroid density in HU is more than 140. In primary hypothyroidism (thyroid hormones are not synthesized) or in diffuse toxic goiter (lack of fixation of thyroid hormone in colloid due to pathological secretion) thyroid density in HU is less than 85 HU. Aim: To demonstrate the necessity of application of thyroid density imaging with computed tomography (CT) for differential diagnosis between iodine-induced hyperthyroidism and non iodine-induced hyperthyroidism.
Materials and methods: Three women with 59, 58, 64-years-old presented for evaluation of tachycardia, nervousness, moderate sweating, weight loss, tremors in the extremities. A 59- year-old woman did not have contact with an excess iodine or bromide. A 58-year-old woman, 18 months ago, had finished treatment with amiodarone. A 64-year-old woman, since a week has been using eye drop (Corvalol) by ophthalmologist’s prescription. All patients were examined clinically and laboratory with determination of hormones – serum TSH and fr.T4, USG of thyroid gland, thyroid scintigraphy with capture index of 99mTc (the ratio of the intensity of radiation (IR) from 99mTc from the zone of interest over the thyroid gland to the IR of the zone of interest over the background on the neck), thyroid density imaging with CT in HU.
Results: The patient’s (59-year-old) clinical and laboratorical values- serum TSH 0.02mU/l (normal value 0.4-4.2 mU/l); fr.T4 64 pmol/l (normal value 9-19 pmol/l); volume of thyroid gland 19 cm3 (normal value till 18 for women); capture index with 99mTc 40 (normal value 2-7); thyroid density in HU 70 (normal value 85-140 HU). The patient’s (58-year-old) clinical and laboratorical values- serum TSH 0.05mU/l (normal value 0.4-4.2 mU/l); fr.T4 21 pmol/l (normal value 9-19 pmol/l); volume of thyroid gland 12 cm3 (normal value till 18 for women); capture index with 99mTc 1.3 (normal value 2-7); thyroid density in HU 150 (normal value 85-140 HU). The patient’s (64-year-old) clinical and laboratorical values- serum TSH 0.28mU/l (normal value 0.4-4.2 mU/l); fr.T4 20 pmol/l (normal value 9-19 pmol/l); volume of thyroid gland 19 cm3 (normal value till 18 for women); capture index with 99mTc 1.5(normal value 2-7); thyroid density in HU 80 (normal value 85- 140 HU).
Conclusion: Among these three patients, increased capture index of 99mTc in thyroid scintigraphy is observed only in one patient (59- year-old), who did not have contact with excess iodine or bromide, but in other two women, capture index is decreased. This decreased capture index indicates that function of iodine trapping has been blocked, due to amiodarone in patient (58-yearold) and carvolol (contains ethylbromoacetate) in patient (64-year-old). Thus, above mentioned clinical presentation demonstrates that 1- Thyroid scintigraphy with 99mTc gives little information in differential diagnosis between Iodine-induced hyperthyroidism and indirectly iodine intake (in form of brome) which might block the function of iodine trapping. This drawback does not allow evaluating adequate function of thyroid gland. 2- Thyroid density in HU with CT is mandatory to use in DD between Iodine-induced hyperthyroidism and indirectly iodine intake. Density variations of TG in HU is 85 to 140 HU is permissible for this diagnosis. When there is iodine-induced impairment of thyroid function, thyroid density in HU is more than 140. In primary hypothyroidism (Thyroid hormones are not synthesized) or in diffuse toxic goiter (lack of fixation of thyroid hormone in colloid due to pathological secretion) thyroid density in HU is less than 85 HU. In accentuation, Iodine consumption, lately, in the form of inorganic or organic pharmacological compounds for therapeutic or diagnostic purposes, has increased. The number of such substances containing different amounts of iodine is more than 29. Patients, often taking them, can’t always remember their names. Despite the existence of a highly effective mechanism for adaptation of TG, excess iodine can cause hyperthyroidism in susceptible individuals. As above mentioned, in hyperthyroidism CT with a measurement of the thyroid density HU for DD is always indicated.
Published Date: 2020-08-01;