Indexed In
- Open J Gate
- JournalTOCs
- The Global Impact Factor (GIF)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
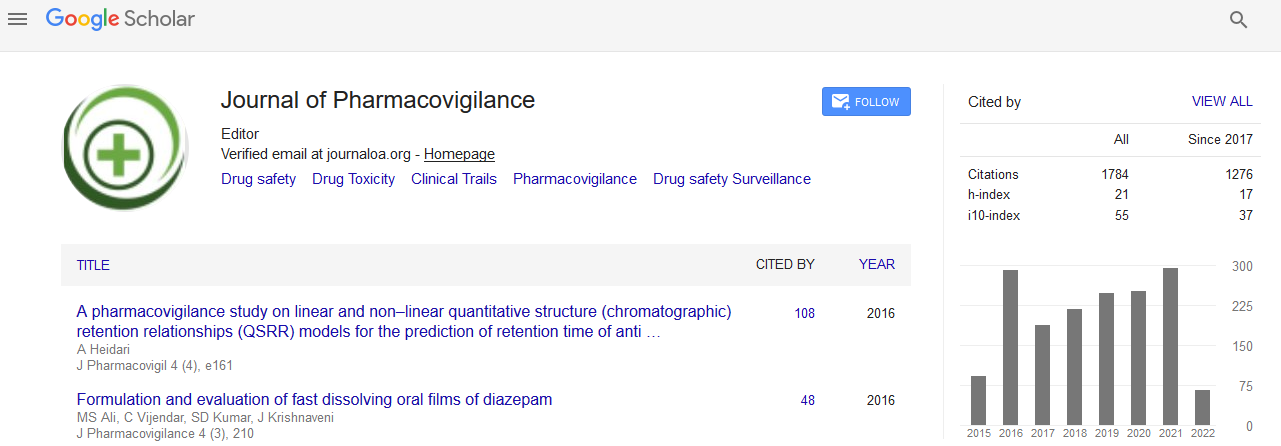
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Dose-Tapering Of TNF Inhibitors in Daily Rheumatology Practice Enables the Maintenance of Clinical Efficacy While Improving Cost-Effectiveness
Dora Pascual-Salcedo, Plasencia Chamaida, Jurado Teresa, L González del Valle, Sabina Prado, Diego Cristina, Villalba Alejandro, Bonilla Gema, Martín Mola Emilio and Balsa Alejandro
Background
The fact that biologics consume a growing portion of health care budget has resulted in an increased attention towards therapy optimization. One of the potential ways to optimize treatment is the down-titration of the administered drug dose.
Objective
To assess whether the clinical activity remains stable after dose tapering of TNF inhibitors in patients with low disease activity and to evaluate the potential benefit of this strategy on the treatment costs.
Method
A cohort of 77 patients with low disease activity treated with TNF inhibitors (TNFi) was monitored. The patients were studied over two time periods: in the 1st period with the drug standard dose, and in the 2nd period with a reduced dose. Clinical efficacy was monitored by DAS28 in rheumatoid arthritis (RA) and by BASDAI in spondyloarthritis (SpA). Serum drug and anti-drug antibody levels were measured by ELISA. The amount of drug dispensed per patient in both periods was compared.
Results
In the 2nd period, although patients received a lower amount of TNF inhibitor, no differences in clinical activity were observed (DAS28 in RA patients: 2.37 ± 0.50 in the 2nd P vs 2.28 ± 0.47 in the 1st P, p=0.20; BASDAI in SpA patients: 1.90 ± 0.93 in the 2nd P vs 1.88 ± 0.95 in the 1st P, p=0.910) and circulating serum trough drug levels were lower (Infliximab: 3.2 ± 2.5 μg/ml in the 1st P vs 1.8 ± 1.5 μg/ml in the 2nd P, p<0.0001; Adalimumab: 5.5 ± 2.8 μg/ml in the 1st P vs 3.1 ± 2.1 μg/ml in the 2nd P, p<0.0001; Etanercept: 1.8 ± 1.1 μg/ml in the 1st P vs 1.3 ± 0.8 μg/ml in the 2nd P p<0.05). The amount of administered drug per patient was reduced in an average of 20% per year.
Conclusion
Dose tapering can be successfully performed in patients with low disease activity, resulting in remarkable savings in the amount of drug used and in the associated costs.