Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
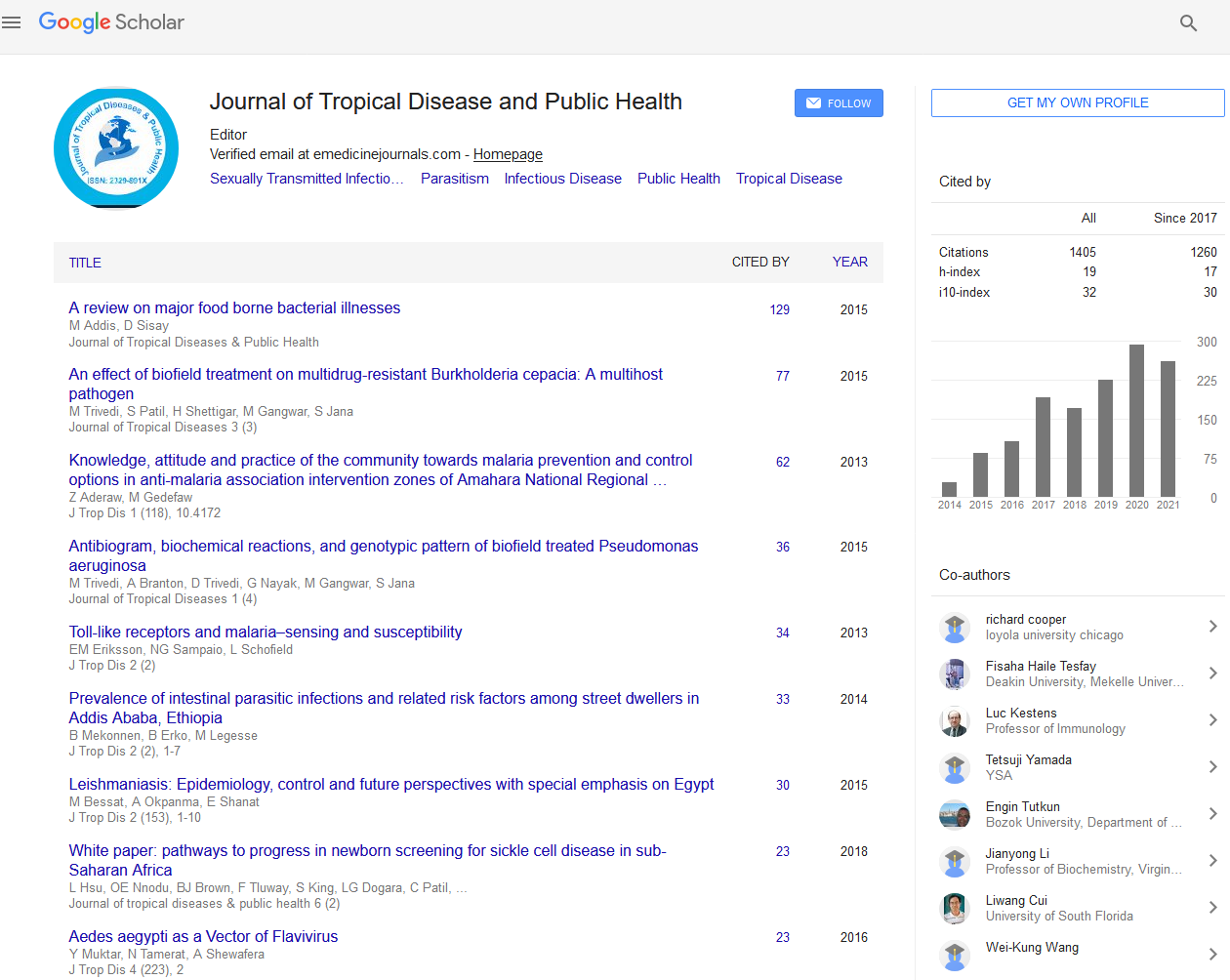
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Dengue Epidemic in Jamshedpur-Tata Main Hospital(TMH) Experience
Sangita Kamath, Neeraj Jain, Satish Gupta, A C Jha and B S Rao
Background: Dengue is the most rapidly spreading mosquito-borne viral disease in the world. There have been few case reports on the clinical and laboratory data in patients with dengue from the eastern part of the subcontinent. Aim: This study was aimed to evaluate the clinical profile and laboratory data of patients admitted in TMH, Jamshedpur in order to understand better the clinical pattern and severity of the disease and to identify the factors associated with bad outcome. Methods: A retrospective study of the case records of confirmed dengue fever cases admitted to the medical wards of TMH, Jamshedpur (Jharkhand), from September to December 2013 was done. The data analyzed included demographic profile, clinical presentation, biochemical parameters, hematological profile, treatment strategy and clinical outcomes. Results: A total of 431 patients were studied. The clinical features observed in this study in the order of frequency were fever (81%), vomiting (43%), myalgias (38%), headache (37%), abdominal pain (15%), haemorrahagic manifestations (15%), skin rash (13%), diarrhoea (12%), ascites (3%), and polyserositis (3%), pleural effusion (2.8%) and hepatomegaly (1.8%). Atypical presentations observed were encephalitis, acute pancreatitis and ARDS. Gastrointestinal bleeding in the form of melaena and hematemesis were the most common haemorrhagic manifestations seen. Thrombocytopenia followed by leucopenia was the most common haematological abnormality found. Severity of thrombocytopenia directly correlated to the haemorrhagic manifestations (P<0.0001) and mortality (P<0.001). Hepatic dysfunction was seen in 40 (9%) patients which included all 16 patients of DHF and 4 patients of DSS. The case-fatality rate observed was 8(1.9%) patients. Deaths were due to disseminated intravascular coagulation (DIC), acute kidney failure, Acute Respiratory Distress Syndrome (ARDS), Multi Organ Dysfunction Syndrome (MODS) and resistant shock. The risk factors that appeared predictive of the bad outcome of the disease and thus of prognostic importance were abdominal pain (RR 8.48, 95% CI 6.36-11.32, P<0.0001), vomiting (RR 1.72, 95% CI .56 to 2.36, P<0.0003), gastrointestinal bleed (RR 10.9, 95% CI 4.8 to 10.62, P<0.0001), thrombocypenia (RR 5.6, 95% CI 3.33- 5.63, P<0.0001), hepatitis (RR 18.57, 95% CI 11.99-28.76, P<0.0001) and ascites (RR 31.42, 95% CI 7.58 to 130.3, P<0.0001) while those associated with increased mortality were hypoalbuminemia (RR-36.8, 95% CI 18.92 to71.2, P<0.0001), transaminitis (RR- 11.21, 95% CI 7.37 to 17.66, P<0.0001), major bleed (RR- 2.99, 95% CI 1.18 to 7.58, P=0.02) and platelet count <50,000/cu mm (RR-2.61, 95% CI 1.27 to 5.36, P=0.01). Conclusion: Fever was the most common clinical presentation in our patients. The spectrum of the disease varied from self-limited viral infection to life- threatening lethal disease. Clinicians should have a high index of suspicion for atypical manifestations. Vomiting, abdominal pain, absence of leucopenia, elevated transaminases; thrombocytopenia and ascites were associated with severe form of the disease and thus can be used as prognostic factors to alert clinician for the prevention of fatal evolution. The mortality can be brought down by high index of suspicion, effective fluid management and strict monitoring.