Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
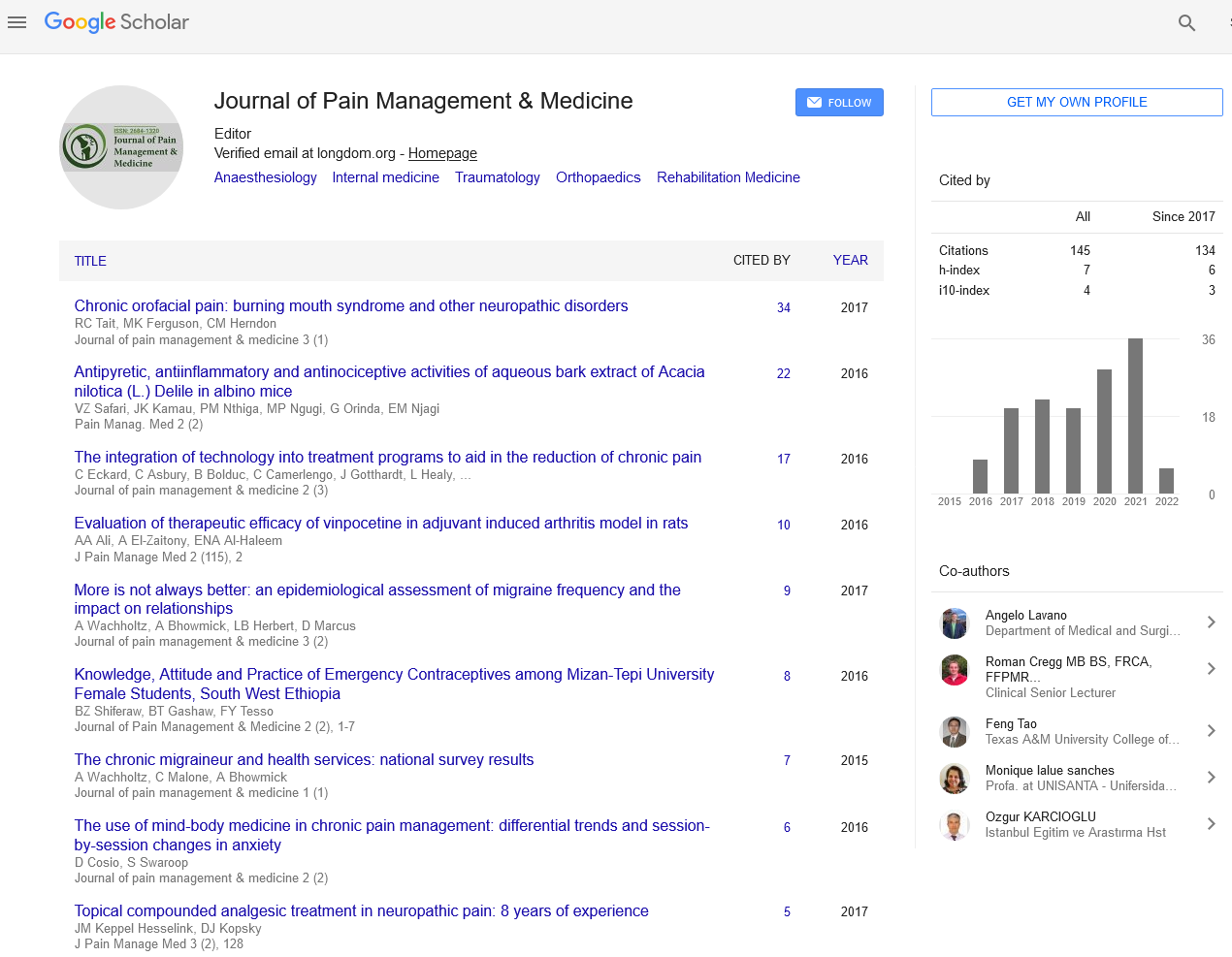
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Continuous Perioperative Thoracic Epidural Fentanyl-Bupivacaine Infusion vs. Continuous Perioperative Fentanyl Intravenous Infusion in Patients Undergoing Major Upper Abdominal Cancer Surgeries
Elzohry AAM, Abd-El-moniem Bakr M, Mostafa GM, Mohamad MF and Ahmed EH
Background: Major upper gastrointestinal cancer surgeries induce postoperative pain, that if not controlled may cause various organ dysfunctions and prolonged hospital and ICU stay. Thus an appropriate pain therapy to those patients must be applicated.
Objective: To compares the effects of continuous perioperative thoracic epidural Fentanyl-bupivacaine infusion versus continuous perioperative Fentanyl intravenous infusion in patients undergoing major upper gastrointestinal cancer surgery.
Methods: 60 patients (ASA II) of either sex were scheduled for elective upper gastrointestinal cancer surgeries. Patients were allocated randomly into two groups (30 patients each) to receive: continuous peri-operative epidural infusion with bupivacaine 0.132 and fentanyl (TEA group), or continuous peri-operative intravenous infusion with fentanyl (control group). Postoperative pain was assessed over 72 h using visual analogue scale (VAS). The intra and post-operative haemodynamic, sedation score and overall patient fentanyl consumption were recorded. Any concomitant events like nausea; vomiting, pruritus or respiratory complications were recorded postoperatively.
Results: There was a significant decrease in pain sensation in TEA group during first day postoperative. Patient haemodynamics was significantly decreased in TEA group. As regard sedation scale, patients of the TEA group were significantly less sedated than control group at immediate postoperative only.
Conclusion: Continuous perioperative thoracic epidural Fentanyl-bupivacaine infusion was much better in pain relief, less sedating effect and shorter duration of hospital and ICU stay than continuous perioperative fentanyl intravenous infusion in patients undergoing major upper gastrointestinal cancer surgery.