Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- Publons
- MIAR
- Euro Pub
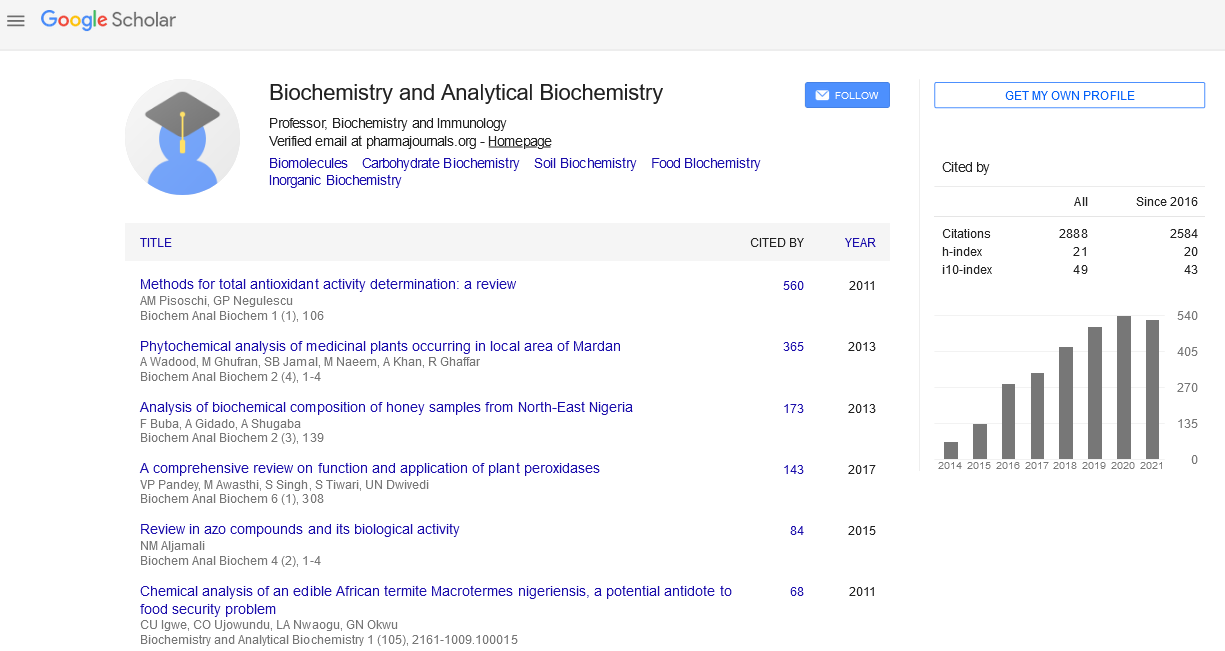
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Blood Transfusion Utility During Cardiopulmonary Bypass and Correlation with Key-Biochemical Laboratory Findings: A New Approach to Identify Preventive and Risk Factors (1-Year Practice at University Hospital Hassan-II of Fez)
El-Hilali F, El-Hilali H, Dheeb BI, Traore BM, Messouak M, Mazouz H, Moumni M, Belgacem FBM and El-Mowafy AM
Background: Blood transfusion (BT) can be mandated during cardiopulmonary bypass (CPB)-aided surgery, although it poses a risk for morbidity and mortality. However, inconsistent BT-strategies have long been documented among clinical settings; thereby limiting its prognostic utility and an evidence-based rational decision there-from.
Methods: Accordingly, we investigated the incidence of BT during (CPB) in 105 cardiac-patients and further assessed its impact/association with demographic data, clinical history data, key biochemical-laboratory findings, inhospital outcomes, incidence of hemofiltration and CPB parameters. Statistical significance and correlations were determined with the SPSS-program-package.
Results/conclusion: 12% of patients received RBC-transfusion during CPB. Parametric analyses indicated significant association between BT and preoperative urea, preoperative creatinine, post-operative urea, and Nadirhematocrit% during CPB. Furthermore, non-parametric Chi-square analysis positively associated BT with combined-surgery, coronary surgery and hemofiltration. Lastly, logistic regression analysis identified Nadirhematocrit value on CPB to inversely correlate with (a negative predictor of) BT, while the history of coronary surgery was found to positively associate with (a risk-factor of) BT during CPB. Thus, BT decision during CPB should be individualized based on weighing the risk/benefits anticipated with anemia and BT and assessing the impact of engaged variables. In this context, while many determinants coexist, Nadir hematocrit and incidence of coronary surgery stand as crucial triggers of a rational decision on BT during CPB.