Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
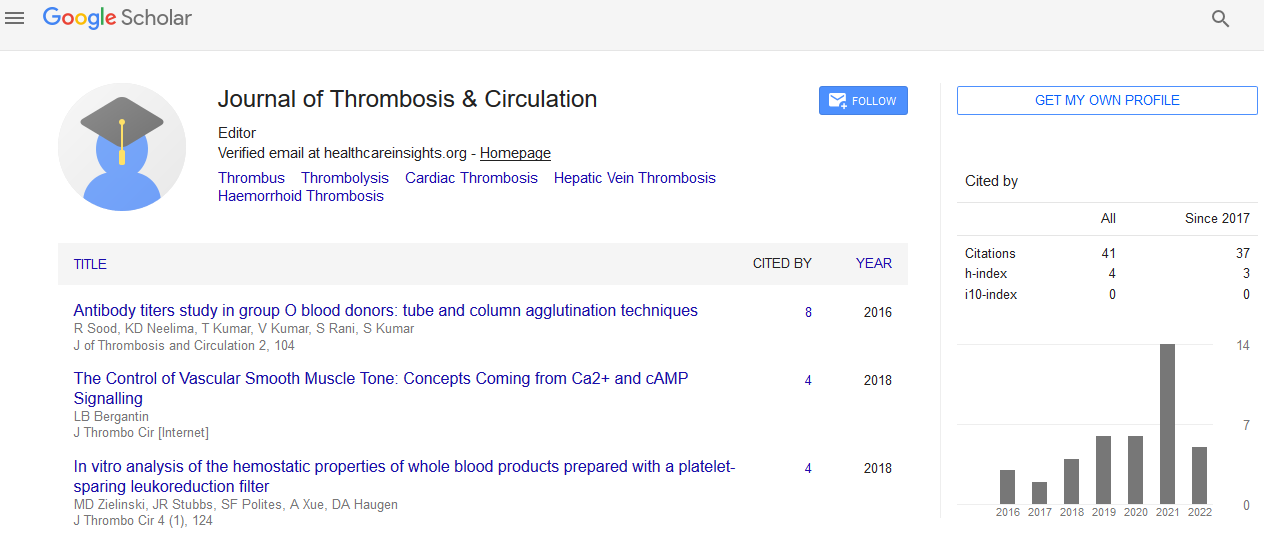
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Association of the C3435T Multi-Drug Resistance Gene-1 (MDR-1) Polymorphism with Clopidogrel Resistance among Moroccan Acute Coronary Syndromes (ACS) Patients
Hind Hassani Idrissi, Wiam Hmimech, Nada El Khorb, Hafid Akoudad, Rachida Habbal and Sellama Nadifi
Background: Antiplatelet drugs are recommended as one of the main medications used in Acute Coronary Syndromes (ACS) patients. However, an inter-individual variability in platelet response to Clopidogrel has been found in a substantial group of them. Genetic is known be the dominant influencing factor for individual and interethnic variations in drug responses. Polymorphisms in the genes involved in Clopidogrel absorption, biotransformation to the active metabolite, or platelet response to adenosine diphosphate (ADP) have been associated to this impaired response. Interestingly, Multi-Drug Resistance gene-1 (MDR-1) polymorphism influences oral bioavailability of clopidogrel and prognosis of ACS patients. The objectives of our study are, first, to determine the frequency of the C3435T MDR1 polymorphism among Moroccan ACS patients compared to healthy subjects; and second, to assess its effect on Clopidogrel response in a sample of Moroccan ASC patients.
Methods and results: 40 ACS patients were recruited and compared to 99 healthy controls. Extracted DNA samples were genotyped by PCR-RFLP method using MboI restriction enzyme. The VerifyNow assay was used to evaluate platelet function among ACS patients. Our results showed that HTA, Smoking, Creatinine and Sex were statistically associated to Clopidogrel resistance (P=0.05; P=0.05; P=0.05 and P=0.04 respectively). 63.64% of the ST (+) patients were carrying the mutant allele, 54.5% of them having the heterozygous genotype and 36.4% the homozygous mutant one, compared to 9.1% having the homozygous wild type genotype. 62.5% of the resistant group was carrying the mutant allele (50% of them had the TT mutant genotype, 25% CT and 25% CC profiles). Among cases, 42.5% were homozygous mutant TT, 35% CC and 22.5% CT, compared to 39.4% CC, 51.5% CT and 9.1% TT among healthy controls. This polymorphism was positively correlated to ACS risk of development in the CT genotype and the additive transmission model (OR [95% CI]=0.49 [0.16-0.99], P=0.002; OR [95% CI]=2.17 [0.94-2.72], P=0.02), increasing-thus- the association of this polymorphism with the risk of pathology occurrence.
Conclusion: To the best of our knowledge, our study is the first in Morocco to assess the effect of the C3435T MDR1 polymorphism on Clopidogrel response in a sample of Moroccan ACS patients; we also tried to explore the frequency of this polymorphism among Moroccan ACS patients and compare them to healthy individuals. The distribution of the mutant allele in Clopidogrel resistance groups, among ACS sub-types, and also in cases compared to controls and there correlations, suggest a potential association of this variant with Clopidogrel resistance and ACS occurrence risk in our population. Understanding the functional and clinical consequences of this MDR1 variant and others may provide a basis for treating patients more effectively. If this variability in response could be assigned to a mutation in the MDR1 gene, patients could be screened and appropriate dose adjustments could be made on the basis of their MDR1 genotype.