Indexed In
- Open J Gate
- JournalTOCs
- The Global Impact Factor (GIF)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
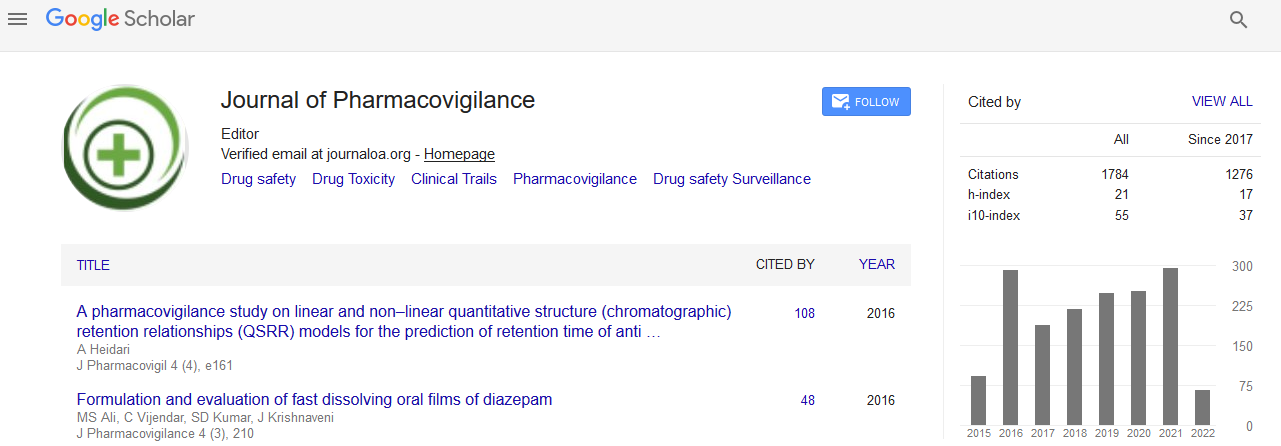
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
A Situational Analysis of Pharmacovigilance System in Republic of Benin
Aurel Constant Allabi and Jude Nwokike
Background: To date, no investigation has been carried out to systematically assess pharmacovigilance systems including quality control and resistance monitoring of artemisinin based combination therapies (ACTs) and other essential medicines in Benin.
Objective: To assess Benin’s pharmacovigilance system, identify the gaps and define elements of strategy which could lead to successful establishment of a functional system in Benin.
Methods: Quantitative approach using structure questionnaires was applied to investigate physicians, pharmacists and pharmaceutical industry representatives’ knowledge, attitude and practice regarding Adverse Drug Reactions (ADRs) reporting and the pharmacovigilance system in Benin. Specific questions examining the ADRs related to ACTs were also asked. Questions regarding reasons for non-reporting and important factors in a decision to report were also addressed.
The Indicator-based Pharmacovigilance Assessment Tool (IPAT) developed by the USAID-funded Strengthening Pharmaceutical Systems (SPS) program was also used to assess the current landscape with different stakeholders. Collecting data on the IPAT indicators was performed during different interviews of key informants. Reviewing documents from different stakeholders was done as well.
Results: All physicians and pharmacists have suspected at least one occurrence of ADR in their practice. 30.77% physicians and 31.11% pharmacists acknowledged that they faced at least one time ADRs suspected to be associated with antimalarial drug treatment (P-value<0.01). However none of the physicians or the pharmacists have ever reported ADRs to the national pharmacovigilance service. Significant difference (Chi2, P<0.05) was found between the proportion of physicians and pharmacists trained in pharmacovigilance (20% versus 1%). The main reasons for not reporting were ‘‘yellow card not available’’ and “not aware about the existence of pharmacovigilance center”.
A small percentage (6.97%) of representatives of the pharmaceutical companies in the country monitors the safety of their products and none of them have ever reported ADRs to the health authority (DPM). In return, none of the laboratories have ever received a report related to quality or ADRs related to their drugs on the market from LNCQ or DMP.
Use of the IPAT tool led to these respective overall scores for core and supplementary indicators: 10 and 7 demonstrating that there is no functional pharmacovigilance system in place. Using these findings, a SWOT analysis was done. The major shortcoming is the lack of expertise in pharmacovigilance despite the availability of qualified human resource in the country. Several recommendations were also made with respect to critical immediate next steps to be taken to ensure that pharmacovigilance and medicine safety systems are developed and sustained in Benin.
Conclusions: This study has helped identify some of the critical challenges and barriers to promoting pharmacovigilance including control of quality and monitoring of ACTs resistance in Benin. There is a need to identify and implement adequate human resources use in order to build capacity and sustain the drug safety system for essential medicines and ACTs in particular. The Ministry of Health should involve all relevant stakeholders including the Faculty of Medicine and researchers to discuss these strategies and develop interventions for the successful implementation of pharmacovigilance in Benin.