Indexed In
- The Global Impact Factor (GIF)
- CiteFactor
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Virtual Library of Biology (vifabio)
- International committee of medical journals editors (ICMJE)
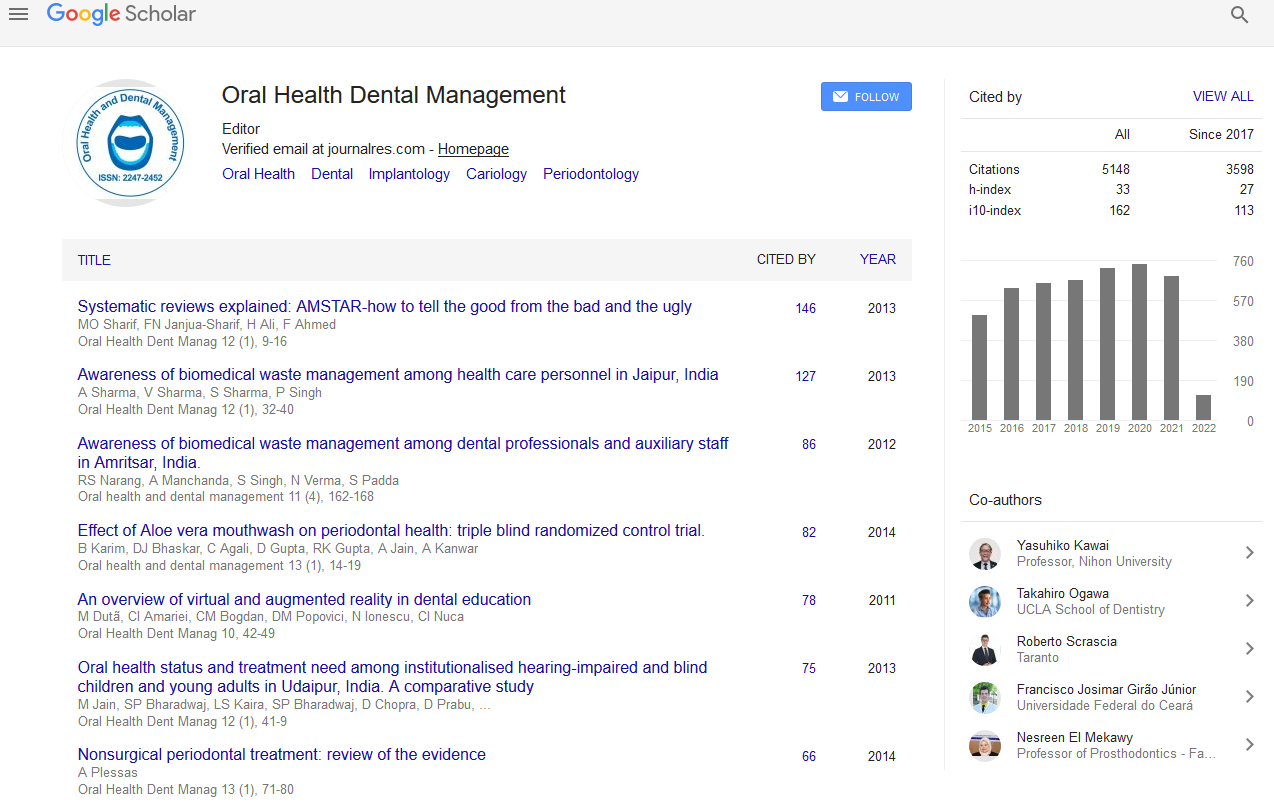
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
A Single Injection Straight Line Approach to Anesthetize Inferior Alveolar Nerve, Long Buccal Nerve and Lingual Nerve: A New Technique
Ahmed Suhael, Tabassum Nafeesa, youssef Sara, Al dayel Omar
Pain management is central to the success of any dental procedure. Many patients choose their dentist based on perceived ability of the dentist to deliver painless dentistry. Inferior alveolar nerve block is the most commonly employed nerve block in mandibular region. Although several techniques for inferior alveolar nerve block have been advocated by various authors, effective anesthesia of the inferior alveolar nerve on a consistent basis is never an easy task particularly for inexperienced dentists. The difficulty usually LIES in the accurate localization of anatomical landmarks particularly the pterygomandibular raphe. It is also a known fact that mandibular anesthetic techniques present a lower success rate when compared to maxillary anaesthetic techniques due to greater density of the mandibular alveolar bone, limited access to the inferior alveolar nerve, marked anatomical variations, and need for deeper needle penetration into the soft tissue. Unfortunately, this nerve block has a comparatively high failure rate. In this article, we present a modification of the conventional inferior alveolar nerve block technique which is simple, easy to master, has high success rate and comfortable to patients as multiple needle penetrations are avoided. In the standard technique, following anesthesia of inferior alveolar nerve, the needle is redirected for lingual nerve anesthesia leading to potential complications which is avoided in single injection straight line technique. A clinical study of alternative inferior alveolar nerve block along with long buccal and lingual nerve blocks, by injecting local anesthesia into the pterygomandibular space by single penetration without redirecting the needle was performed on two hundred and seven patients undergoing simple extractions and surgical extractions of mandibular molars. A success rate of 97.5% was obtained