Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
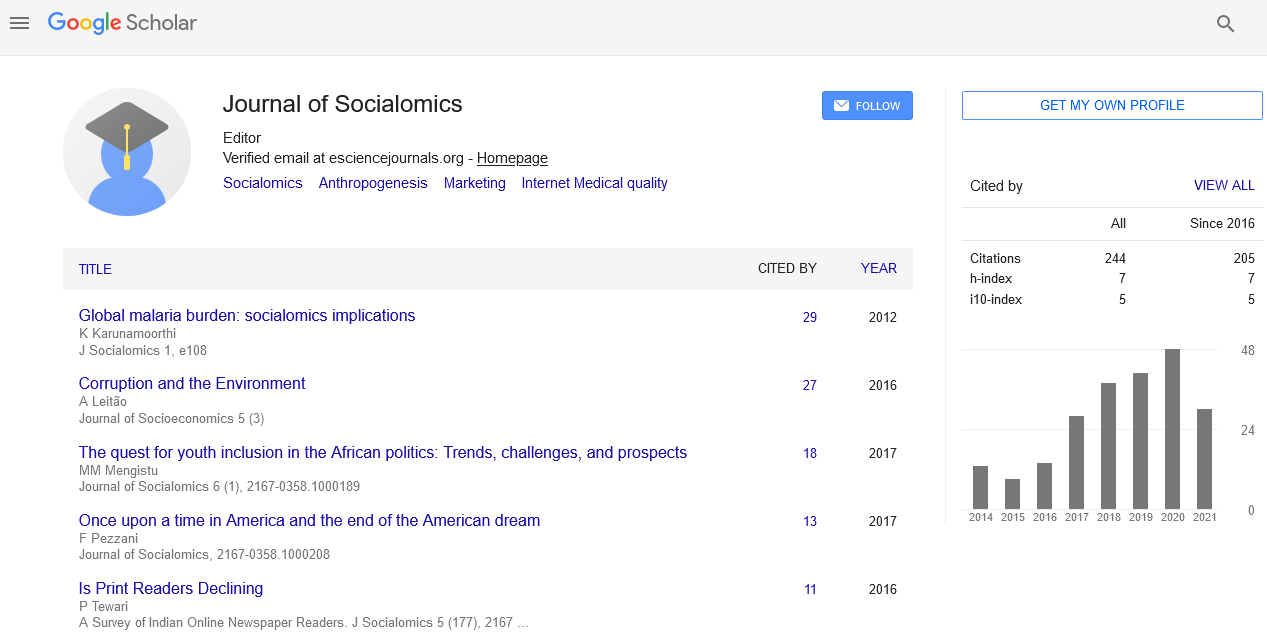
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
A Review of the Literature : How Social Constructs and Cultural Practices Erect Barriers to Facility Deliveries in Rural Nigeria
Jerome Aondona Shaguy*
Nigeria’s population is 2% of the world’s total population, but Nigeria carries 10% of the global maternal mortality burden. In the last 16 years, a combination of Millennium Development Goal 5 and the return of democratic governance in Nigeria has focused a stronger spotlight on the crisis. Nigeria did not meet MDG targets (reducing the incidence of maternal deaths by 75% by 2015). The proximal causes of morbidity/mortality in Nigeria are clinical factors viz: Hemorrhage, sepsis, obstructed labor and complications from unsafe abortions. These factors indicate a systemic weakness in the quality and availability of services. This paradigm has often informed program design. However, recent studies suggest the problem is more complex and thus requires more contextual nuance. Extra clinical factors such as-distance to facility and cost of transportation, decision making power and spiritual and cultural conditioning vis a vis health seeking behavior have all been shown to play a significant role in forming barriers or acting as enablers to better outcomes for maternal morbidity and by extension mortality. Furthermore, social attitudes towards extra-marital pregnancy and subsequent unsafe abortion practices play a highly significant role. This problem is largely a “Northern Nigeria problem”, this region has a much higher burden that the rest of the country, 165/100000 in the South and as much as 1549 in the North. The North of Nigeria is largely disadvantaged with low literacy, poor sanitation, low urbanization and high birth rates [6]. This environment has bred gender related disadvantages and insular social conditioning.
Published Date: 2020-10-29;