Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
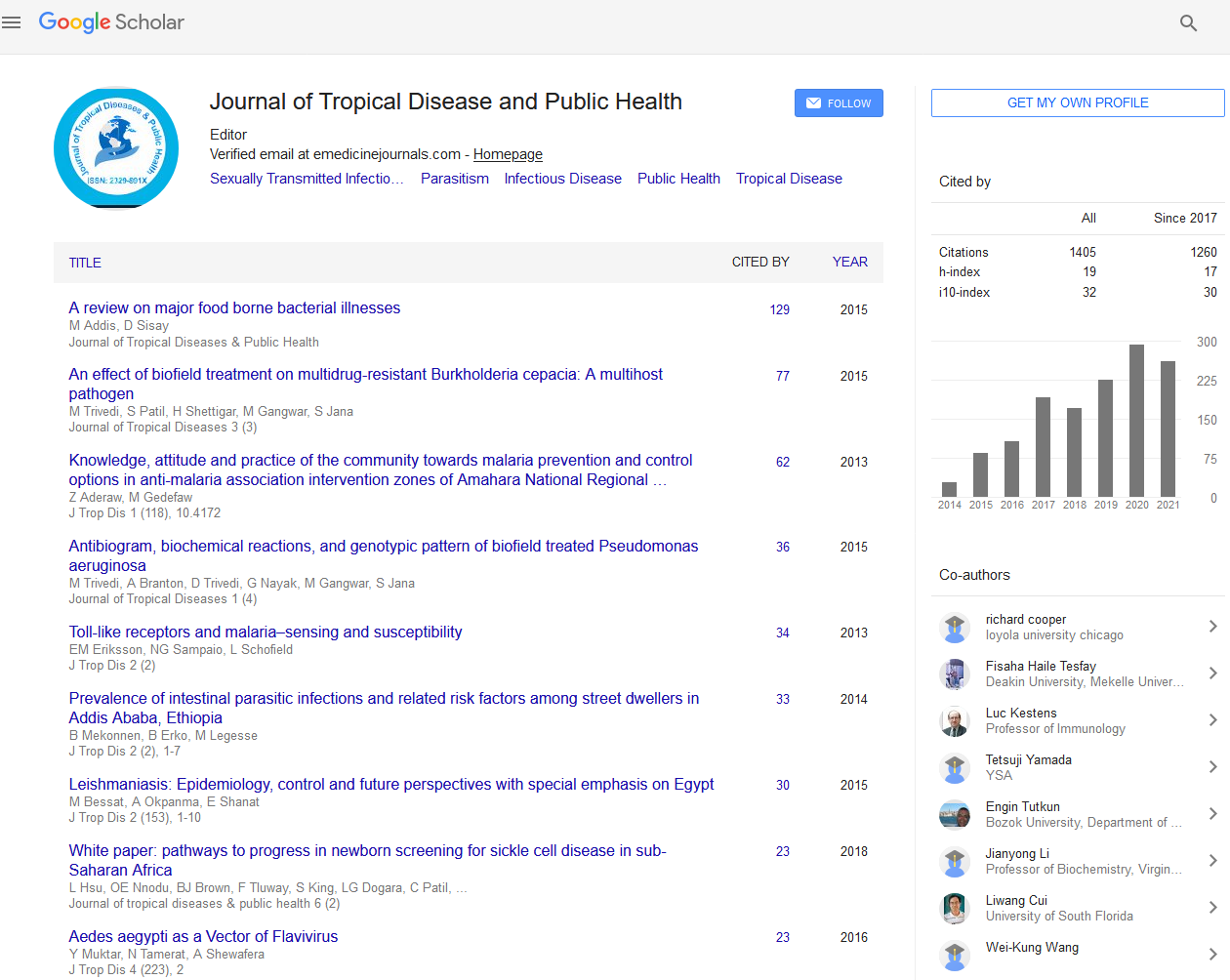
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
A Review of Neonatal Morbidity and Mortality in an Intensive Care Unit of a Paediatric Health Facility in Lagos, Nigeria
Bamgboye M Afolabi, Cecilia O Clement and Victor Inem
Introduction: Neonatal period in developing countries is characterized by various infectious diseases that make up leading causes and significant contributors to dismal morbidity and mortality statistics in this period of life. The diagnosis of neonatal sepsis in sub-Saharan Africa represents a challenge due to unavailability or scarcity of laboratory aids. The clinical diagnosis of sepsis may be difficult without laboratory aids irrespective of where the infant is born due to the fact that other non-infectious conditions can present with sepsis-like picture.
Objectives: The main objectives of this study were to document frequently diagnosed illnesses, record the management of the ill neonates and present the leading causes of death during the neonatal period for the purpose of future planning.
Methodology: This was a retrospective review of the medical records of children admitted into the Intensive Care Unit (ICU) of a public health facility between March 2005 and February 2007. Descriptive analysis was used to illustrate findings. The study was conducted between March 31, 2009 and June 30, 2009.
Results: Majority (135, 60.3%) of the study neonates (135 males, 89 females) were aged between 2-7 days. In all, 46 (20.5%) neonates weighed less than 2.5 kg. There was a considerable difference (t=-2.45; p=0.015; CI -0.60, -0.06) in the mean (± SEM) body temperature of 24-hour old neonates (36.7 ± 0.11) compared with those 2-7 days old (37.1 ± 0.06). Fever (56, 44%) was the most frequent presentation among neonates diagnosed with septicaemia (126, 56.3%), yellowness of the eyes (47, 65.3%) among those diagnosed with jaundice (72, 32.1%) and failure to cry (9, 25.7%) among those diagnosed with birth asphyxia (35, 15.6%). Full blood count was the most frequent (207, 92.4%) investigation requested for while antibiotics was the commonest (461, 205.8%) medication prescribed. Medications were administered to the neonates mainly through the intravenous route (538, 240.2%). In all, mortality among the studied neonates was 76 (33.9%).
Conclusion: More effective measures to improve neonatal mortality could be 1) improving access to antenatal care provided by trained medical professionals 2) giving general instructions to mothers who just gave birth regarding when to seek medical attention for her newborn infant 3) assessing local professional competencies 4) reviewing obstetrical procedures and interventions around the time of labour for women who deliver in hospital/private clinic settings, etc. For example appropriate chemoprophylaxis of pregnant mothers colonized with Group B Strep (GBS) proved to be a very effective prophylactic measure for early-onset neonatal GBS sepsis.