PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
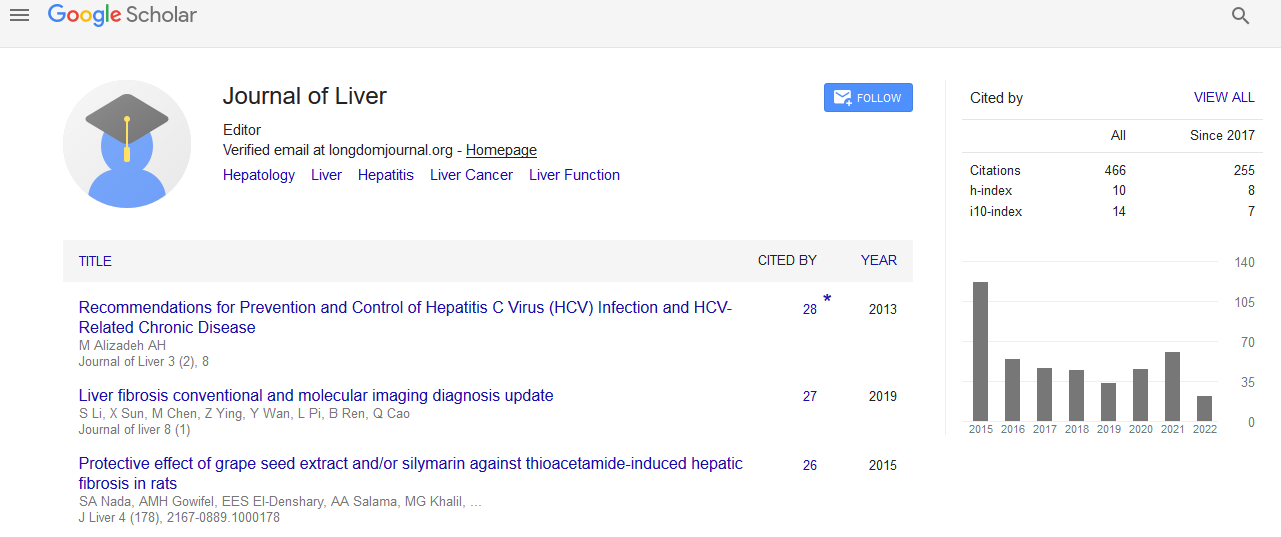
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
A Rare Cause of Biliary Obstruction
Kian Makipour, Alexandra Modiri and Houshang Makipour
Objective: To discuss a rare cause of obstructive jaundice. Methods: A case report is presented with emphasis on diagnosis and management. Six month follow up is also presented.
Results: A 42 year old African-American male presented with one week of painless jaundice. He underwent imaging via CT abdomen pancreatic protocol and MRCP demonstrating a massively dilated common bile duct of 12 cm and diffuse intrahepatic ductal dilation. He subsequently developed pruritus, RUQ abdominal pain, and cholangitis thus necessitating an endoscopic retrograde cholangiopancreatography (ERCP). ERCP was performed but not useful in delineating the biliary tree anatomy or relieving biliary obstruction. Later percutaneous transhepatic cholangiography (PTC) was performed to provide drainage and was also not useful in delineating his biliary tree anatomy. Shortly thereafter he underwent laparotomy, choledochal cyst and bile duct resection, Roux en Y pancreaticojejunostomy and hepaticojejunostomy. A review of the pathologic specimen indicates the presence of intrapapillary neoplasm of the bile duct (IPNB) which is a rare variant of a bile duct tumor. The specimen was positive for MUC1 and CEA which indicates a high possibility of recurrence.
Conclusions: Invasive carcinoma has been found to be present in 70-80% of cases of resected IPNB. However, survival has been shown to be better in patients with IPNB compared to those with conventional bile duct tumors. Given the difficulty of preoperative diagnosis of these lesions and their high predisposition for invasion all IPNB should be surgically resected.